Introduction
There has been significant pressure to modernize the software in the healthcare sector. Medical facilities are expecting new functionalities, such as:
- Integration with national e-health systems
- Telemedicine capabilities
- Dedicated patient portals for accessing test results or scheduling appointments
At the same time, the architecture of many systems implemented when these needs didn’t exist, can significantly complicate the introduction of such changes.
This becomes particularly challenging when the system has been implemented in multiple medical facilities. Every architectural change must be carefully planned and executed to avoid disrupting the daily work of medical professionals. Moreover, medical facilities often use different versions of the system, which further complicates the modernization process.
A complete system replacement is rarely a viable option – it presents too much business and operational risk, especially with large-scale implementations.
Fortunately, there are proven modernization strategies that allow for gradual adaptation of existing systems to contemporary requirements while maintaining operational continuity for clients.
Two Proven Modernization Strategies
The industry literature and practice recognize two strategies for modernizing legacy systems in the medical sector. These approaches are well-tested and documented.
The key to success lies in properly adapting them to the specific case, taking into account the technical and organizational conditions of the given system.
Strategy 1: Internal API Implementation
The first approach involves expanding the existing system with an API layer directly within its structure. This is a deep integration that uses the native capabilities of the source technology to implement modern interfaces compliant with interoperability standards.
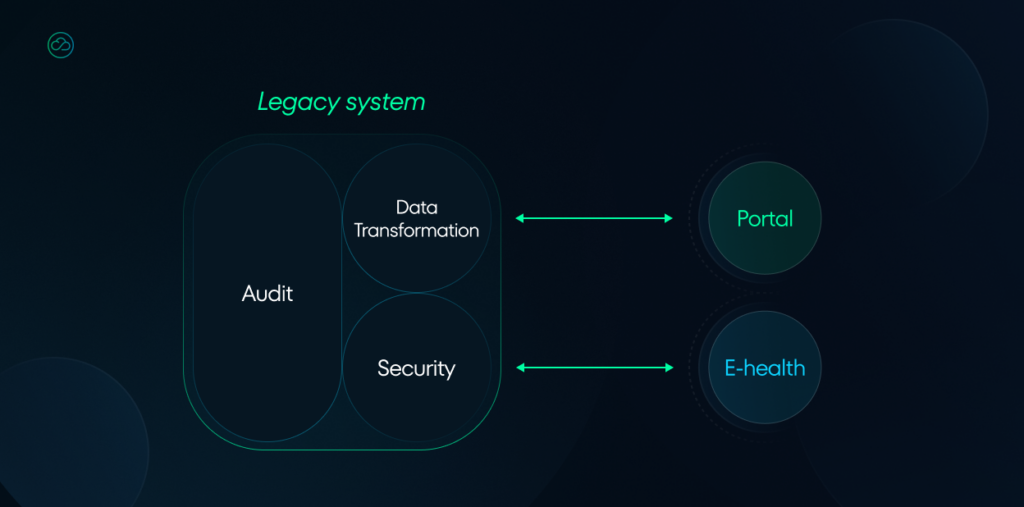
Technical implementation in this case includes:
- Implementing a data transformation layer between the legacy model and standard format (e.g., FHIR Resources).
- Adding RESTful API endpoints supporting appropriate HTTP methods.
- Implementing authentication and authorization mechanisms compliant with OAuth 2.0/OpenID Connect.
- Implementing medical terminology validation and mapping mechanisms.
Key aspects & challenges:
- Direct access to the data persistence layer.
- Ability to use native transaction mechanisms.
- Lower data access latency.
- Possible but difficult to achieve consistency with existing security mechanisms.
- Difficult to add newer mechanisms such as caching and monitoring due to lack of libraries and frameworks.
Strategy 2: External API Connector
The second approach involves creating an independent middleware layer using a modern technology stack, which acts as an adapter between the legacy system and the external world. The connector functions as a standalone application, responsible for retrieving data from the source system, transforming it into standard formats, and making it available through modern API interfaces.
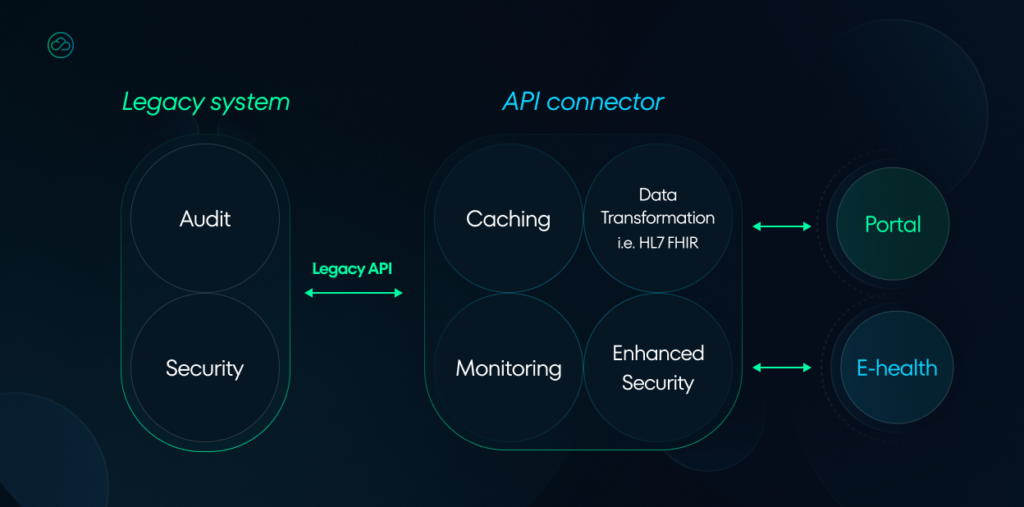
The technical architecture of the connector includes:
- Integration layer with the source system (through available interfaces or direct database access).
- Data transformation engine with complex structure mapping support.
- Implementation of standard REST/FHIR interfaces.
- Data caching and buffering layer.
- Asynchronous operation queuing system.
- Monitoring and logging module.
- Failover and error handling mechanisms.
Technical aspects to consider:
- Choosing an appropriate technology stack (e.g., Spring Boot, Node.js).
- Implementing integration patterns (Circuit Breaker, Bulkhead).
- Managing data consistency between systems.
- Optimizing performance and scalability.
- Implementing retry and error compensation mechanisms.
Practical Example
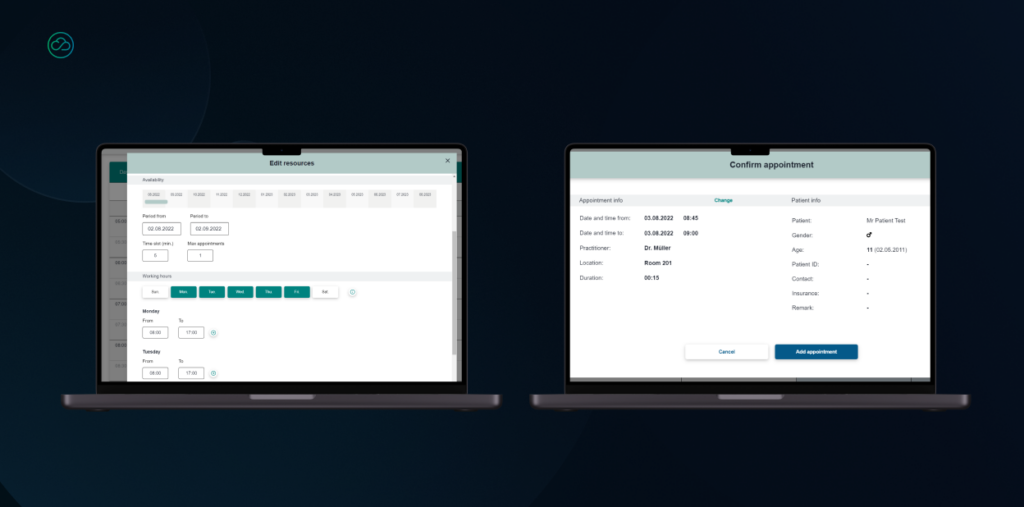
Recently, we faced the challenge of modernizing an appointment scheduling system in a hospital. The facility wanted to enable patients to self-register online, but the existing system lacked appropriate interfaces.
In this case, we applied the external API connector strategy. We created a modern middleware layer that:
- Retrieves available appointment data from the legacy system
- Transforms it into a standard format based on HL7 FHIR resources
- Makes it available through REST API
- Synchronizes changes in real-time
We developed a web-based solution using React JS for the frontend, building a completely new GUI layer that maintained visual consistency with the original system while opening it up to external access. The interface was designed with responsive principles, ensuring seamless operation across all devices.
The backend was built with .NET, connected to a PostgreSQL database. To ensure reliability and scalability, we implemented a high-availability architecture and containerized the entire solution using Docker.
Thanks to this solution, the hospital gained a modern patient portal while retaining its proven backend system.
The use of HL7 FHIR standards for the information model also positioned the system well for future integrations with other healthcare platforms.
Why Invest in Modernization?
Modernizing selected system components, instead of complete replacement, brings three key benefits.

1. Investment optimization while maintaining business value
Modernizing a selected system component requires significantly less financial and organizational resources than comprehensive replacement, while still meeting specific business needs.
For example, adding online self-registration capabilities for patients doesn’t require replacing the entire facility management system – it’s sufficient to modernize the appointment management module. We achieve the same business value at a much lower cost.
2. Enhanced security and reliability
Using modern technologies in modernized components not only raises security levels but also increases the entire system’s resilience to failures.
With components more loosely connected, potential problems in one part of the system have limited impact on other modules. While managing multiple distributed components requires appropriate competencies and tools, the separation resulting from the architecture significantly reduces the risk of cascading system failures.
3. Part of a long-term modernization strategy
Gradual modernization of individual components can be part of a broader strategy for modernizing the entire facility’s IT system.
This evolutionary approach allows for better distribution of resources over time, risk minimization, and the opportunity to learn from experiences in earlier stages. Moreover, modernized components can serve as a “proof of concept” for broader changes, providing concrete evidence of modernization benefits.
Summary
Healthcare system modernization is a complex issue requiring deep knowledge of both technical aspects and healthcare sector specifics. Choosing the appropriate strategy – whether internal API implementation or external connector – should be preceded by a thorough analysis of the specific case.
In our practice, we’ve found that the key to success is combining experience in legacy system modernization with knowledge of the latest interoperability standards and healthcare sector specifics.
Collaboration with an experienced technology partner not only helps minimize risk but also maximizes the potential of existing systems during their modernization process.
Considering system modernization or partial upgrades?
We’re happy to share our experiences and help analyze available options. We invite you to a technology consultation, during which we will:
- Analyze your current system architecture
- Discuss your business needs
- Propose optimal technical solutions
- Estimate potential risks and costs
Click the button below and leave your contact details, and we’ll get in touch with you about an online meeting.
