Introduction
It’s no secret that data is the foundation of medicine today. The growing popularity of EHR systems has meant that we gain more and more of this information, which is critical to quality healthcare. According to some sources, the average hospital generates 50 petabytes of data per year, or nearly 137 terabytes per day. This number continues to grow, according to some sources by as much as half a year per year!
Such a large amount of constantly emerging data is a tremendous resource, creating unprecedented opportunities for treatment and optimization of this process (e.g., using AI). On the other hand, it places additional responsibilities on medical facilities to secure and organize this information so that it can be used at all. Unfortunately, the vast majority of this data is not usable. According to World Economic Forum, we effectively use only about 3% of the available data.
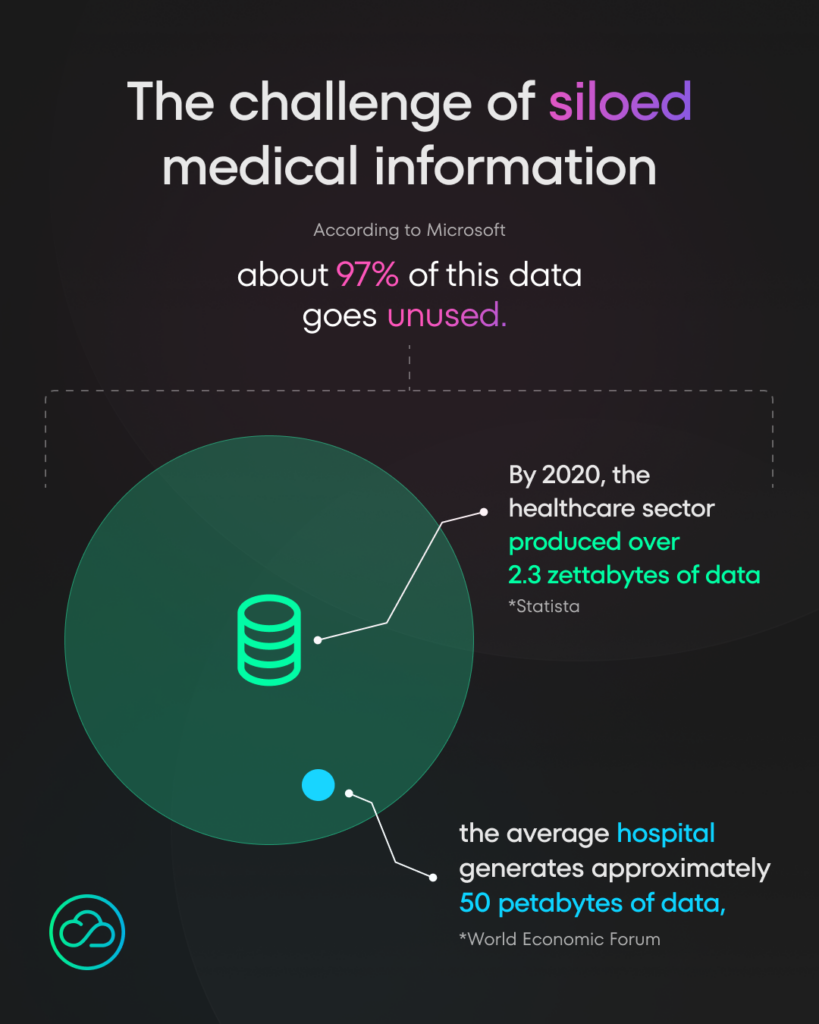
To increase that number, there have been many efforts over the years to make data structured and, more importantly, interoperable.
But what does interoperability even mean, especially in healthcare? What are the barriers to achieving it? What are the basic standards of medical data and for what purpose should they be used?
The following article will help you get started with interoperability and provide answers to all of these questions!
What is interoperability?
At its core, data interoperability in healthcare is about enabling seamless communication and data exchange between different information systems, devices, and applications. It’s the ability of health information systems to work together within and across organizational boundaries to advance the effective delivery of healthcare for individuals and communities.
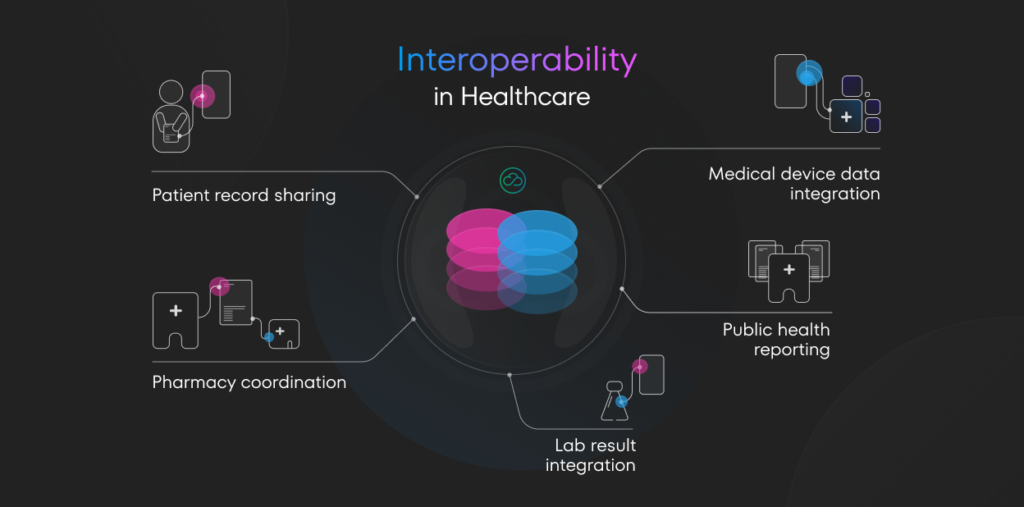
Let’s break this down with some specific examples of how seamless interoperability may look like:
- Patient record sharing — interoperability allows a primary care physician’s electronic health record (EHR) system to share a patient’s medical history, allergies, and current medications with a specialist’s EHR system in a different hospital. This ensures the specialist has all relevant information for the patient’s care.
- Lab result integration — when a patient gets a blood test at a laboratory, interoperability enables the results to be automatically sent to and integrated into the patient’s record in their doctor’s EHR system, regardless of whether the lab and the doctor use systems from different vendors.
- Pharmacy coordination — interoperability allows a doctor’s e-prescribing system to communicate directly with a pharmacy’s system, sending prescription details securely and accurately, reducing errors and improving efficiency.
- Medical device data integration — in a hospital setting, interoperability enables data from various medical devices (like heart rate monitors, ventilators, or infusion pumps) to be automatically recorded in the patient’s EHR, providing a real-time, comprehensive view of the patient’s condition.
- Public health reporting — interoperability facilitates automatic reporting of notifiable diseases from healthcare providers to public health agencies, enabling faster response to potential outbreaks.
Why interoperability matters?
The benefits of achieving data interoperability in healthcare are far-reaching and potentially transformative. It leads to improved patient care and outcomes by providing healthcare providers with access to complete medical histories, enabling more informed decisions and reducing medical errors.
This is crucial given that an estimated 12 million Americans experience diagnostic errors in primary care settings annually, and 40,000 to 80,000 deaths occur each year in US hospitals due to misdiagnosis. The need for interoperability is further highlighted by the fact that over 35% of Medicare beneficiaries see five or more physicians annually.
Interoperability also enhances efficiency and reduces costs by eliminating manual data entry and streamlining information access. This is significant considering that for example, in the US, the healthcare system wastes approximately $600 billion annually due to fraud, waste, and abuse. Despite spending about $4 trillion on healthcare annually, the highest in the world, US life expectancy has dropped by two years since 2019.
Recognizing the importance of interoperability, 55% of health system Chief Information Officers anticipate increasing spending on interoperability measures in 2023 compared to 2022, demonstrating a growing commitment to addressing this critical challenge in healthcare.
4 biggest challenges in healthcare data management
Data silos
Despite its importance, achieving true data interoperability in healthcare remains a significant challenge. The sector is plagued by fragmented systems and data silos, where valuable patient information is locked away in disparate databases that cannot communicate effectively with one another. This fragmentation is often the result of years of piecemeal technology adoption, leading to a patchwork of systems that weren’t designed to work together.
Poor interoperability
The scale of this problem is staggering. According to recent studies, 60% of health systems receive duplicate, incomplete, and junk data from other healthcare organizations, highlighting the poor quality of data exchanged between systems. Furthermore, 69% of health organizations struggle to integrate data from external sources, indicating widespread difficulties in achieving true interoperability.
Legacy systems
Legacy systems pose another major hurdle. Many healthcare organizations still rely on outdated technology that lacks the capability to integrate with modern systems. These legacy systems often use proprietary data formats, like Cerner CCL or Epic Chronicles, making it difficult to extract and share information without significant effort and cost.
Data security
It may sound paradoxical, but the way medical information is legally protected severely limits its free use. According to some sources, medical data is worth far more than financial data (e.g., credit card information) on the dark web. While protecting this data should remain a priority, we should find a way to use it in a secure, privacy-compliant manner, in accordance with regulations such as HIPAA in the United States or GDPR in Europe.
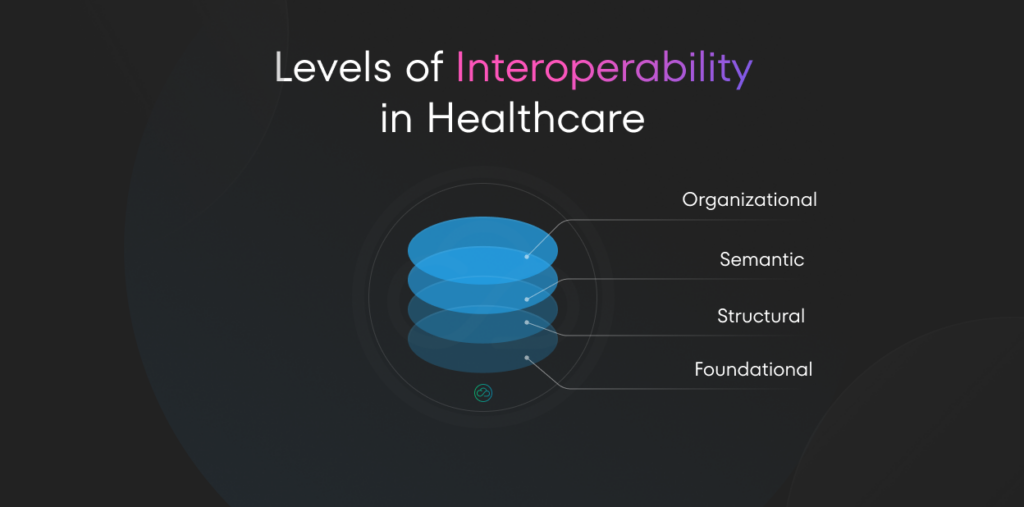
The Four Levels of Interoperability
When discussing healthcare interoperability, it’s important to know that it exists on a spectrum, typically defined by four distinct levels. Understanding these levels is crucial because achieving true interoperability in healthcare requires progress across all four:
Level 1 – Foundational Interoperability
- This is the most basic level, allowing data exchange from one information system to another without requiring the receiving system to interpret the data. It establishes the interconnectivity requirements needed for one system or application to communicate data to and receive data from another securely.
Level 2 – Structural Interoperability
- At this level, the format of data exchange is defined. It ensures the uniformity of data movement from one system to another, preserving its clinical or operational purpose and meaning. This level defines the syntax of the data exchange and ensures that data can be interpreted at the data field level.
Level 3 – Semantic Interoperability
- This level ensures that both systems can understand the data in the same way, interpreting the meaning of the data exchanged. It allows for the seamless sharing and interpretation of data across systems, ensuring that the meaning of the information is preserved and understood as it moves from system to system.
Level 4 – Organizational Interoperability
- The highest level of interoperability, this encompasses the broader scope of governance, policy, social, legal, and organizational considerations to facilitate the secure, seamless and timely communication and use of data within and between organizations and individuals. It involves complex issues of trust and policy to enable widespread data sharing and usage.
While many current efforts focus on structural and semantic interoperability, reaching organizational interoperability is the ultimate goal for a fully integrated healthcare system.
Semantic interoperability, in particular, is a key component. It ensures that the meaning of the data is preserved across systems. This goes beyond just transferring data; it involves making sure that the data is interpreted correctly in different contexts. For instance, ensuring that a diagnosis code means the same thing across different healthcare providers and systems.
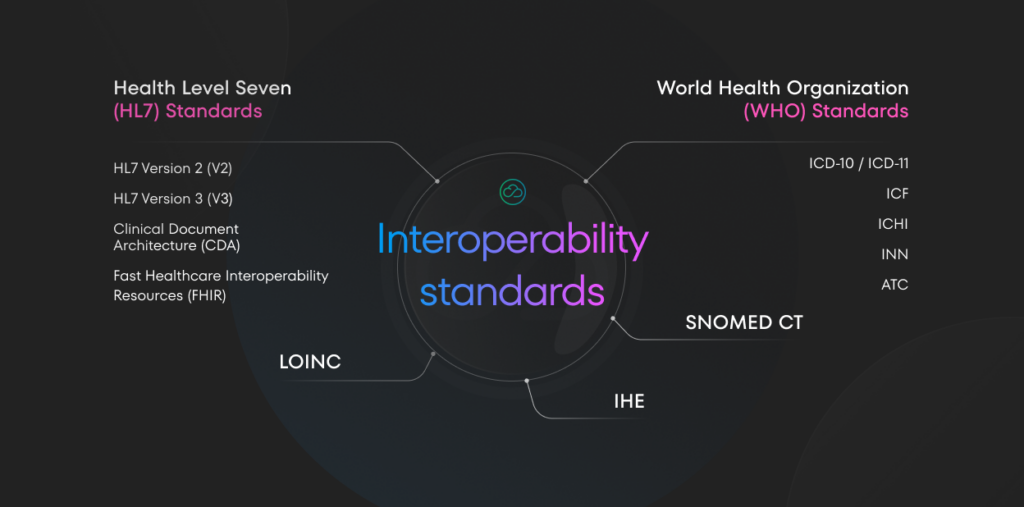
Medical Standards – The Interoperability Foundation
Alright, now that we’ve got a handle on what interoperability is, how important it is, and what the levels of interoperability are, let’s move on to the equally important issue – interoperable standards and protocols. This is the foundation for data exchange and integration.
Interoperable health standards define how health information should be structured, exchanged, and interpreted. These standards are crucial in ensuring that data can be shared and understood across different systems and organizations.
Let’s explore some of the most important standards:
Health Level Seven (HL7) Standards
HL7 is a set of international standards for transferring clinical and administrative data between software applications. It includes:
- HL7 Version 2 (V2): One of the most widely used standards for exchanging healthcare data. It’s particularly common in hospital settings for transmitting patient data.
- HL7 Version 3 (V3): A more comprehensive standard that uses an XML-based structure. While more robust than V2, its complexity has limited its adoption.
- Clinical Document Architecture (CDA): A standard for specifying the structure and semantics of clinical documents for exchange.
- Fast Healthcare Interoperability Resources (FHIR): The newest HL7 standard, designed to be easier to implement than V3 while addressing the limitations of V2. FHIR uses modern web technologies and is gaining rapid adoption.
SNOMED CT (Systematized Nomenclature of Medicine — Clinical Terms)
SNOMED CT is a comprehensive, multilingual clinical healthcare terminology. It provides a standardized way to represent clinical phrases captured by the clinician and enables automatic interpretation of these. This is crucial for semantic interoperability, ensuring that the meaning of clinical terms is consistently understood across different systems.
IHE (Integrating the Healthcare Enterprise)
IHE is not a standard itself, but rather an initiative that creates detailed implementation guides (called profiles) on how to use established standards to solve specific clinical and operational needs. It promotes coordinated use of established standards like DICOM and HL7 to address specific clinical needs.
DICOM (Digital Imaging and Communications in Medicine)
DICOM is the international standard for medical images and related information. It defines the formats for medical images that can be exchanged with the data and quality necessary for clinical use. This standard ensures that medical imaging equipment from different manufacturers can work together seamlessly.
LOINC (Logical Observation Identifiers Names and Codes)
LOINC provides a set of universal names and ID codes for identifying health measurements, observations, and documents. It’s particularly important for lab test results, allowing different systems to understand and interpret these results consistently.
World Health Organization (WHO) Standards
WHO provides several important standards used globally:
- International Classification of Diseases (ICD-10 / ICD-11): These are the foundation for identifying health trends and statistics globally. ICD-10 is widely used, while ICD-11 is the latest version, incorporating significant updates.
- International Classification of Functioning, Disability and Health (ICF): This classification of health and health-related domains helps to measure health and disability at both individual and population levels.
- International Classification of Health Interventions (ICHI): A common tool for reporting and analyzing health interventions for statistical purposes.
- International Nonproprietary Names (INN): A unique name given to a pharmaceutical substance that is globally recognized.
- Anatomical Therapeutic Chemical (ATC) Classification System: Used for the classification of active ingredients of drugs according to the organ or system on which they act and their therapeutic, pharmacological, and chemical properties.
These standards form the foundation of healthcare interoperability.
By providing common languages and structures for health data, they enable different systems to exchange information meaningfully. However, implementing these standards effectively across diverse healthcare ecosystems remains a significant challenge.
The role of government and industry initiatives
Governments and industry bodies play a significant role in promoting healthcare interoperability. Many countries have launched national e-health initiatives aimed at creating standardized, interoperable health information systems.
These initiatives often involve setting up health information exchanges and promoting the adoption of electronic health records.
Several countries have made significant strides in implementing national e-health services:
Germany 🇩🇪
In Germany, the state of informatization of healthcare at the national level is advanced, with several key initiatives implemented to enhance digital health services. The entity responsible for setting the standards of work in the health sector is ‘Gematik‘.
Here are some of the key initiatives:
- ePA (Elektronische Patientenakte) – a digital platform provided by health insurers that allows patients to store and access all their health data, such as test results and medical reports, via an app, ensuring comprehensive and centralized management of medical documents.
- KIM (Kommunikation im Medizinwesen) – a secure email service designed for healthcare providers to communicate sensitive patient information securely.
- TIM (Telematikinfrastruktur Messenger) – a secure messenger service for healthcare professionals to exchange information and coordinate care.
- e-Rezept (Elektronisches Rezept) – enables the digital issuance and processing of prescriptions, allowing patients to receive prescriptions electronically and pharmacies to process them efficiently.
- NFDM (Notfalldatenmanagement) – Provides quick access to critical emergency data, such as allergies and medications, stored on the electronic health card.
- eAU (Elektronische Arbeitsunfähigkeitsbescheinigung) – a digital system for issuing and managing sick leave certificates.
- eGK (Elektronische Gesundheitskarte – Electronic Health Card): A mandatory health insurance card that stores essential personal data, emergency information, and provides access to digital health services.
Gematik’s role in detailing these standards ensures interoperability, security, and efficiency in the digital transformation of Germany’s healthcare system.
We wrote some articles about Germany healthcare system:
- E-prescription – how does it actually work?
- 4 Challenges for software vendors while implementing e-prescription in Germany
- What is CardLink and why is it so important?
Poland 🇵🇱
In Poland, the state of informatization of healthcare at the national level is progressively advancing, with several key initiatives implemented to enhance digital health services. The entity responsible for setting the standards of work in the health sector is the e-Health Centre (Centrum e-Zdrowia).
Here are some of the key initiatives:
- IKP (Internet Patient Account): A digital platform provided by health insurers that allows patients to store and access all their health data, such as test results and medical reports, via an app, ensuring comprehensive and centralized management of medical documents.
- e-Recepta (E-prescription): Enables the digital issuance and processing of prescriptions, allowing patients to receive prescriptions electronically and pharmacies to process them efficiently.
- e-Skierowanie (E-referral): A digital system for issuing and managing referrals to specialists and medical services, improving efficiency and reducing paperwork.
- e-ZLA (Electronic Sick Leave Certificate): A digital system for issuing and managing sick leave certificates.
- eWUŚ (Electronic Verification of Beneficiary Entitlements): A system for verifying patients’ insurance status in real-time, ensuring eligibility for healthcare services.
- P1 Platform: A nationwide healthcare information exchange platform that integrates various e-health services and systems, facilitating the secure sharing of medical data between healthcare providers.
- EDM/ZM (Electronic Medical Documentation/Medical Events): A system that digitizes medical records and tracks all medical events and interactions a patient has within the healthcare system, providing a comprehensive history of patient care.
The Centre for Health Information Systems (CSIOZ) plays a crucial role in detailing these standards, ensuring interoperability, security, and efficiency in the digital transformation of Poland’s healthcare system.
PS. If you want to learn more about national Polish healthcare system, read our article about it here: E-Services in the Polish Healthcare Sector
By providing a standardized framework and shared infrastructure, these initiatives can significantly accelerate progress towards a more connected, efficient healthcare system. Both Germany and Poland demonstrate how national e-health strategies can drive the adoption of interoperable systems, improving patient care and healthcare efficiency.
Conclusion: The Path Forward
Recognizing the critical importance of interoperability, the healthcare industry is beginning to act. In 2023, over half of health system Chief Information Officers anticipate increasing their spending on interoperability measures.
Technology plays a crucial role in improving interoperability within healthcare systems.
The following technological advancements are key to achieving true interoperability:
- Advanced data standards – the implementation of standards like HL7 FHIR, SNOMED CT, and LOINC provides a common language for healthcare data, facilitating seamless information exchange.
- Artificial Intelligence – AI and Machine Learning technologies can significantly enhance the ability to interpret and standardize data from disparate sources, improving interoperability.
- Blockchain – blockchain technology offers a secure and transparent way to share health data across different organizations while maintaining patient privacy.
- Cloud-based solutions – cloud computing provides scalable and flexible platforms for storing and sharing healthcare data, making it easier for different systems to connect and exchange information.
- API-First architectures – developing systems with robust APIs (Application Programming Interfaces) from the ground up allows for easier integration and data exchange between different healthcare IT systems.
By focusing on these technological solutions, healthcare organizations can significantly improve their interoperability, leading to better patient care, increased efficiency, and reduced costs.
As health issues increasingly cross borders, the adoption of these technologies on an international scale becomes ever more important for achieving global health interoperability.
Who we are?
At NubiSoft, we are proud to be part of this transformative journey, contributing our expertise and innovative solutions to shape the future of healthcare interoperability. As we look ahead, we remain committed to driving progress in this vital field, ensuring that the benefits of interconnected health systems reach patients and providers worldwide.
Seeking expertise in data interoperability, medical data standardization, or healthcare e-services?
Contact us to discuss potential collaborations and mutual opportunities.